Valvular Heart Disease and Heart Failure
In humans, there are four one-way valves within the heart. These are called the aortic and mitral valves, located on the left side of the heart, with the pulmonary and tricuspid valves located on the right side of the heart. Structurally, the tricuspid valve separates the right atrium from the right ventricle, the mitral valve separates the left atrium from the left ventricle, the pulmonary valve lies between the right ventricle and pulmonary artery and the aortic valve between the left ventricle and the aorta.
Animation |
|
 |
How the normal heart works |
Valvular Heart Disease (VHD) can be defined as a disease process involving one or more of the four valves of the heart.
Animation |
|
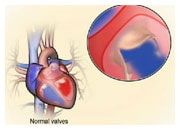 |
How abnormal heart valves can cause heart failure |
Valves can become damaged as a natural consequence of ageing, or due to rheumatic heart disease, or a bacterial infection affecting the valves or as a consequence of a congenital abnormality. In some parts of the world (e.g. Africa), VHD is one of the most common causes of heart failure, whereas in Europe and America, VHD is a rather rare cause of heart failure. However, any abnormality that affects the functioning of the valves may lead to the development of heart failure. In patients with heart failure and a weakened heart muscle (reduced ejection fraction), enlargement and dilatation of heart cavities can lead to distortion and abnormality of the heart valves. This abnormal function is usually leakage of blood through the mitral and tricuspid valves, leading to worsening symptoms, such as shortness of breath.
Irrespective of the cause leading to VHD, alterations to the valve can result in one or both of the following conditions: 1. valve insufficiency (often referred to as valve regurgitation) whereby the valve in unable to prevent the backflow of blood due to the leaflets of the valve not correctly connecting ; 2. valve stenosis which is a narrowing of the valvular opening, therefore blocking an adequate outflow of blood, which is particularly noticeable on exercise, as the heart cannot increase the flow of blood required. Insufficiency and/or stenosis can affect any of the four heart valves.
Careful evaluation of the individual patient’s history and symptoms followed by physical examination with special attention to heart auscultation with a stethoscope are key initial steps in the diagnosis of VHD. Echocardiography is considered the gold standard for VHD imaging, diagnosis and assessment of valve function. Additional imaging modalities include cardiac magnetic resonance (CMR) and computed tomography (CT).
The three types of valve problems most commonly seen in heart failure are briefly discussed below.
Aortic stenosis is characterized by a thickening of the valvular ring or leaflets (typically due to calcification) impairing the ability of the left ventricle to eject blood into the aorta which then travels around the rest of the body. As a result, the work of the heart muscle increases leading to thickening, similar to the situation with high blood pressure. Aortic stenosis occurs most commonly in the elderly. Typical symptoms are shortness of breath, angina (chest pain) and syncope (fainting). Classification of the disease severity along with treatment decisions are based on echocardiography. In patients with no symptoms and mild-moderate aortic stenosis, regular clinical and echocardiographic assessment are recommended. For patients who are symptomatic and /or have severe disease of the valve (defined as a valve area less than 1 cm2), either standard aortic valve replacement (open-heart surgery) or trans-catheter aortic valve replacement (TAVR) is recommended. TAVR is a minimally invasive intervention which does not require open-heart surgery. The artificial valve is delivered to the heart using a cardiac catheter and therefore is recommended for certain patients, especially those who would be high-risk for standard surgical aortic valve replacement (i.e. elderly).
Aortic regurgitation is caused by a leakage of blood through of the aortic valve back into the left ventricle. As a consequence, the left ventricular cavity dilates, and the cardiac muscle is forced to work harder to eject more blood. Patients experience symptoms of heart failure (typically shortness of breath, palpitations, angina). Severity classification is based on echocardiographic assessment. Aortic valve repair or replacement (open-heart surgery) is recommended in symptomatic patients with severe aortic regurgitation and in patients that are asymptomatic but have evidence of weakened left ventricle (reduced ejection fraction). Patients with mild to moderate aortic regurgitation should be followed with regular clinical assessment and echocardiography.
Mitral insufficiency is the most common VHD and is due to an inability of the mitral valve to close properly when the heart pumps blood out from the left ventricle into the aorta. As a consequence, there is an abnormal leakage of blood backwards into the left atrium (regurgitation). Mitral regurgitation can be either caused by disease of the mitral valve itself or by dilatation of the left ventricular cavity as a consequence of heart failure. Typically, patients present with increasing symptoms of heart failure. Echocardiography is used to assess the severity of the leakage. This is based on an evaluation of the volume of blood flowing backwards (or regurgitated) into the left atrium. In symptomatic patients with primary disease of the mitral valve and severe regurgitation, surgery (mitral valve repair or replacement) is recommended.
In patients with heart failure and secondary mitral regurgitation optimal medical therapy for heart failure is essential and may be effective in reducing symptoms. Recently, catheter-based, edge-to-edge repair for secondary mitral regurgitation has been developed and may be a low-risk option in symptomatic patients with heart failure and severe mitral regurgitation. In practice, the most common procedure is called MitraClip. This minimally invasive procedure (which does not require open-heart surgery) is based on the delivery of a special device (the Mitraclip) via blood vessels in the groin. First to the right side of the heart and then into the left side of the heart. The Mitraclip is then positioned over the leaky mitral valve using the delivery system which substantially reduces or eliminates the mitral regurgitation. Various other techniques are currently being tested in clinical trials.
Patients who have been informed that there is a problem with one of the valves in their heart will have many questions and need sufficient time to understand the consequences of the problem and discuss potential treatment options. Adequate information and support should be provided by healthcare professionals.