Beta blockers
What they do
When your heart is not pumping as well as it should, your body will try to compensate by producing adrenaline and noradrenaline, hormones that cause the heart to beat faster and increase blood pressure. If this effect is prolonged, it can have harmful effects on a heart that is already struggling to work effectively. Beta blockers help your heart beat more slowly and lower your blood pressure, thus protecting your heart from the harmful effects of prolonged adrenaline and noradrenaline activity.
Beta blockers are an important part of managing heart failure. However, people with moderate or severe heart failure may need to start with a low dose, which is then increased slowly. This is because some people may experience a temporary increase in their heart failure symptoms during the first few weeks of beta blocker treatment.
What are the expected benefits?
Beta blockers have been shown to reduce heart failure-related hospitalisations, prolong life, and improve exercise tolerance and quality of life.
Side effects
Beta blockers slow down the heart rate and lower the blood pressure. Therefore, they may also mildly reduce your tolerance to exercise (exercise capacity). This means that you may feel more tired when you are physically active. However, this initial effect will usually pass when your body systems get used to the medication‘s effects.
Of note, there are certain target doses for each beta blocker, and your doctor may increase your dosage slowly in order to achieve the best benefit for you.
Sometimes, beta blockers can make your hands and feet feel cold. Gloves will help.
Beta blockers may also make asthma worse, so be sure to inform your doctor if you have asthma.
Depression can sometimes occur with some beta blocker therapy. You should discuss any symptoms you have with your nurse or doctor.
Patients suffering from special skin problems like psoriasis should be aware that beta blockers may worsen the condition in some patients.
Top tips
Beta blockers can initially make you feel dizzy and tired as they lower your blood pressure and heart rate. Patients starting beta blocker therapy are recommended to “start low, go slow”. It may take a few weeks for you to feel better after you start taking a beta blocker – but if you still feel dizzy after this time, contact your doctor or nurse to make sure you have been given the right dose.
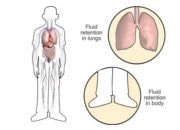
It’s useful to keep track of your weight on a daily basis and contact your doctor or nurse if there are any significant changes.
It is very important that you yourself keep track of your blood pressure, heart rate and weight on a daily basis, e.g. in paper-based format or a digital diary. See the Monitoring Chart which is downloadable under Useful Tools on the home page of this website. Contact your doctor or nurse, if you notice any significant changes.
If you feel very wheezy or short of breath, contact your doctor as this may be due to underlying asthma symptoms.
It’s important that you don’t stop taking your beta blockers suddenly. Any dose reduction or discontinuation of treatment should be discussed with your doctor first.
Also known as:
- Acebutolol
(Sectral®, Prent®) - Atenolol
(Atenix®, Tenormin®) - Bisoprolol
(Soloc®, Vivacor®, Cardicor®, Emcor®, Concor®) - Carvedilol
(Eucardic®, Coreg®) - Celiprolol
(Celectol®) - Labetalol
(Normodyne®, Trandate®, Normozyde®) - Metoprolol
(Betaloc®, Betaloc SA®, Lopressor®, Lopressor LA®, Toprol XL®) - Nadolol
(Corgard®) - Nebivolol
(Nebilet®) - Oxprenolol
(Trasicor®, Slow-Trasicor®) - Pindolol
(Visken®) - Propanolol
(Angilol®, Syprol®, Bedranol SR®, Beta Prograne®, Slo-Pro®, Inderal®, Half-Inderal LA®, Inderal-LA®) - Sotalol
(Beta-Cardone®, Sotocor®) - Timolol
(Betim®) - Combination products
(Co-tenidone®, Kalten®, Tenoret®, Tenoretic®, Viskaldix®, Prestim®, Beta-Adalat®, Tenif®)